 The Coastal Carolina Bariatric surgery program, led by the medical director Dr. Michael “Logan” Rawlins MD, offers the full spectrum of comprehensive medical and surgical weight loss services. Our practice is an accredited center by the American Society for Metabolic and Bariatric Surgery, is a designated Blue Cross Blue Shield Blue Distinction Center, and is an OPTUM Bariatric Center of Excellence. All medical office appointments, endoscopy, and surgery are provided at Summerville Medical Center.
The Coastal Carolina Bariatric surgery program, led by the medical director Dr. Michael “Logan” Rawlins MD, offers the full spectrum of comprehensive medical and surgical weight loss services. Our practice is an accredited center by the American Society for Metabolic and Bariatric Surgery, is a designated Blue Cross Blue Shield Blue Distinction Center, and is an OPTUM Bariatric Center of Excellence. All medical office appointments, endoscopy, and surgery are provided at Summerville Medical Center.
Are you a candidate?
If you have been struggling with obesity for years and have not seen great weight loss success with diet, exercise, and eating behavior changes, bariatric surgery may be a great option for you. You are a candidate for surgery if your BMI (body mass index) is above 35 kg/m2. Use a BMI calculator to determine where you stand.
Obesity is often associated with a multitude of medical conditions that can significantly affect your lifestyle, overall health, and ultimate life span. Not only are we targeting weight loss with the operations, but also improvement or resolution of these medical conditions, including diabetes, high blood pressure, high cholesterol, sleep apnea, reflux/GERD, heart disease, fatty liver, PCOS and joint pain. Bariatric surgery has been shown in studies to be the only reliable method for substantial and durable long-term weight loss. If you are at least 100-150 pounds overweight, it is unlikely you will be able to lose enough weight with just diet, exercise, and/or medications; that is where surgery is most beneficial.
The workup process
The first step is to watch our free online informational session to learn more about the surgical options, requirements, workup process, post-op diet and long-term follow-up. You should then call the office at (843) 875-8994 to schedule a new patient appointment with the bariatric surgeon, Dr. Rawlins, to discuss your personal medical history, interest in surgery, and any questions you may have.
You will also meet with our dietician who will assess your current eating habits and establish a plan for you moving forward to eat better. Our clinic will also call your insurance company to verify that you have bariatric surgery coverage and benefits. Most insurance plans will cover the surgery minus your copays or out-of-pocket expenses, but a few insurance plans do not cover bariatrics; in that case, we will discuss options for self-pay programs with you. At the initial visit with the surgeon you will be given a checklist of items to complete for the surgical workup. This includes labs, EKG, upper endoscopy (EGD), and psychological clearance; you will also be required to complete a three to six-month insurance physician-supervised diet and eating behavior counseling program, which is done through our office. Additionally, you might need a sleep study, cardiology heart clearance or other medical testing as indicated. Once this workup process is complete, you will be scheduled for your surgery date. Our program will help guide you along the way through each step to make sure you stay on track.
After surgery
The typical hospital stay after bariatric surgery is one or two nights. When you go home from surgery, you will remain on a liquid diet for a few weeks, then transition to soft, squishy foods, and eventually resume solid food after a month out. This slow diet transition is necessary as your stomach heals. You are encouraged to walk as much as possible but will not be cleared to resume full unrestricted activity till after one month. You can return to work or school whenever you feel able; for sedentary or desk jobs, that could be in as little as 2-3 weeks, or for heavy lifting or manual labor jobs, more like four to six weeks. Our clinic will see you for follow-up visits after surgery at two weeks, four weeks, three months, six months, 12 months, and then yearly; these visits are very important to track your weight loss and make sure no problems are developing.
Dietary and exercise changes
Dietary and exercise changes are absolutely necessary both before and after surgery in order to be successful. While the operations are very helpful in reducing weight loss early after surgery, maximal weight loss achievement and long-term weight maintenance can only be realized by adherence to good dietary habits. If dietary habits are not changed, weight regain is likely; you do not want to squander all your hard work. You should view surgery as a jump start or reset button that will help get you over the hill and achieve the weight loss success you have always been looking for. However, once you are 12 months out from surgery, your body makes adjustments, weight loss slows down or stops, and long-term weight maintenance has very little to do with the surgery and everything to do with your eating behaviors and movement. We will be there to coach you along every step of the way.
Bariatric surgery operations
Our center performs the most common operations done in the country, which include the Sleeve Gastrectomy and Gastric Bypass, as well as some less common operations like the Duodenal Switch and SADI (single anastomosis duodenal switch). We also perform complex revision surgery to fix or enhance previous operations and conversion surgery to change from one operation to another, usually for inadequate weight loss or weight regain. All of the operations work by restricting the amount of food you can intake, which lessens overall calories and alters the gut hormones that affect your body’s metabolism, food storage, and hunger levels. Some operations also involve intestinal re-arrangement to limit food absorption.
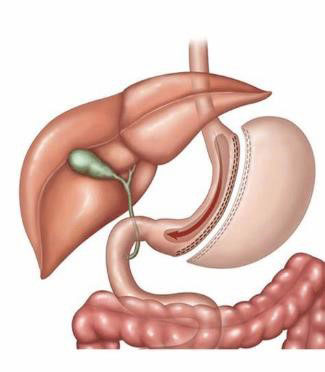
Sleeve gastrectomy – In the “Sleeve,” we remove 80 percent of the excess stomach you don’t need in order to restrict food intake while leaving the rest of the bowel alone. This maintains the normal anatomic continuity of how you eat while providing a smaller stomach to make you feel full much faster. It is the quickest and easiest of the operations to perform with the least number of long-term complications and is the most common operation performed in the country. You can expect to lose at least 50-60% of your excess weight but it could be more based on your starting BMI and adherence to the post-operative diet and exercise requirements. Worsening reflux and weight regain are the most common issues seen in the long term.
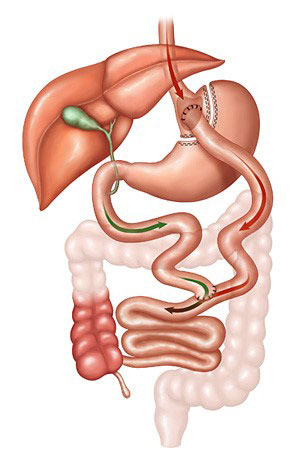
Gastric bypass – Also referred to as the “Roux-en-Y” due to the configuration of the anatomy, in this operation, we divide your stomach to make a small pouch about the size of an egg or two, which provides the restrictive effect, and then we rearrange your small bowel to bypass the rest of the stomach and a portion of the small bowel to limit food absorption. This operation is considered to be the “gold standard” bariatric operation that has been around for the longest period of time, and as other operations have come and gone over time, this one has always stuck around. It provides reliable and consistent weight loss, helping you lose about 60-80% of your excess weight. The anatomy is a little more complex than the sleeve so the operation takes a little longer to perform, but the post-operative course is the same. There are more long-term complications to worry about, such as marginal ulcers, internal hernia, intussusception, and vitamin/nutrient deficiency. Due to the upper anastomosis of the stomach to the small bowel, there is a risk of ulcers forming at this connection, which can be caused by smoking/nicotine, NSAIDS (like ibuprofen), and steroids; thus, all of these must be avoided completely specifically after gastric bypass surgery. For patients with bad reflux/GERD who are obese, the gastric bypass is the preferred surgery as it will provide the best relief of reflux symptoms.
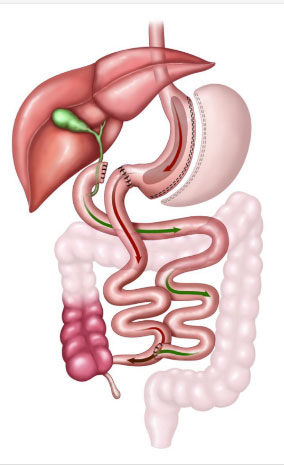
Duodenal switch and SADI – The duodenal switch is similar to combining a sleeve and a gastric bypass with a few modifications. Part of the stomach is removed just like a sleeve, and the small bowel is also rearranged like a gastric bypass; however, the upper anastomosis is done to the duodenum and not the stomach and a greater amount of bowel is bypassed. There is also a modification to the duodenal switch called the “SADI,” where only a single upper anastomosis is constructed, which lowers the risk of complications related to the second connection on the more distal bowel. These operations are usually reserved for higher BMI (>50) patients or those seeking conversion from sleeve gastrectomy for inadequate weight loss or weight regain with persistent severe medical conditions related to obesity. With this operation, there is a much higher chance of vitamin and nutrient malabsorption, which requires more vitamin supplementation, more protein intake, frequent lab draws, and close follow-up to make sure these problems are not developing. Weight loss is the best, with >80 percent excess weight loss being common, but this must be balanced with the risk of malnutrition.
Revision surgery – Sometimes, bariatric operations need to be revised to fix a problem related to a previous operation while keeping the expected anatomy of the operation essentially the same. This can be due to a marginal ulcer (which can lead to bleeding, perforation, or obstruction), stricture or narrowing of an anastomosis, fistula, internal hernia, intussusception, reflux and hiatal hernia, gastric pouch or anastomosis dilation, or inadequate bowel bypass for optimal weight loss. Not all practices perform bariatric revision operations as they are more complex surgeries and carry a higher rate of complications, but Dr. Rawlins has extensive experience in this space and feels very comfortable performing and managing these operations.
Conversion surgery – At times, patients may need their bariatric operation converted to a completely different type of operation to aid in better weight loss or relieve a complication. Again, similar to revision surgeries, these operations are more complex and are performed by highly experienced surgeons like Dr. Rawlins. Examples of conversion operations are:
- Lap band to sleeve
- Lap band to gastric bypass
- Sleeve to gastric bypass (for reflux/GERD)
- Sleeve to duodenal switch (for inadequate weight loss)
- Vertical banded gastroplasty (VBG) to gastric bypass (for gastric outlet obstruction)
- Gastric bypass reversal (for marginal ulcer or chronic nausea/intolerance)
Historical (lap band) – Many patients still come to the office asking about the Lap Band. This was a very common operation in the early 2000s but started to fall out of favor around 2010. Patients chose this operation because they did not want their intestines rearranged with a Gastric Bypass and saw this as a more palatable change to their body. In this operation, a plastic adjustable band was placed around the upper stomach that could be made tighter or looser to adjust restriction. Long-term use data has shown us that weight loss is very poor with this operation, and many patients develop reflux/GERD, pain, band slip, band erosion and gastric obstruction; for those reasons, the band would need to be removed. It can be taken out without additional surgery or could be converted to a sleeve or gastric bypass; the bypass is more common as the weight loss results and reflux control is much better.
Medical weight loss drug therapy
Our center not only performs weight loss surgery, but we also offer medical weight loss drug therapy. With the newer class of GLP-1 injectable medications (Ozempic, Wegovy, Mounjaro, Zepbound) becoming very popular, we are now able to expand our reach to treat obesity beyond just surgery. While anyone who is obese is a candidate for these medications, our program uses them in a more targeted way. We will prescribe these medications for patients who are:
- Still contemplating surgery but want to try medications first
- Who need to lose weight before surgery for safety reasons if their starting BMI is too high
- For weight loss stalls or weight regain after surgery
- For patients not a candidate for surgery. The medications can sometimes be hard to find at local pharmacies, or there can be insurance coverage issues that may limit their use in all patients.
Why choose Coastal Carolina Bariatric?
We know you have options in who you choose to see for your healthcare, and patients today are more savvy consumers than ever before. We know you will do your research before trusting your life to another person. Our bariatric director, Dr. Rawlins, truly cares about each and every patient and their journey. He is a thoughtful physician, a good listener and easy to communicate with. Dr. Rawlins has well over a decade of experience in the field of bariatric surgery, having taken care of thousands of weight loss surgery patients. He is board-certified and fellowship-trained in bariatric and general surgery and is the director of a bariatric program that is accredited as an ASMBS Center of Excellence. Dr. Rawlins is also a 14-year active duty Veteran of the United States Air Force, having provided lifesaving care to service members throughout the globe; his life experience and calm demeanor will put you at ease, knowing that the commander in charge is always looking out for you first.
You will also have a surgeon who runs a comprehensive bariatric program that performs all of the major operations to tailor the right surgery for you and a program that offers both medical and surgical weight loss support as well as dietary counseling. Quality, safety, patient satisfaction and good outcomes are at the forefront of our practice. Ultimately, we care about your weight loss journey. This is not just an operation; this is a significant life change, and we will be there for you every step of the way!